Adult Day Services
We care for adults living at home who need daytime assistance for health and safety. Our warm and welcoming adult day centers provide a place to spend the day and find friends, activities, and encouragement. Our staff also coordinates with clients, caregivers, and in some instances, doctors to support every client. We help families stay together!

Adult Day Services
We care for adults living at home who need daytime assistance for health and safety. Our warm and welcoming adult day centers provide a place to spend the day and find friends, activities, and encouragement. Our staff also coordinates with clients, caregivers, and in some instances, doctors, to support every client. We help families stay together!
Cities Served
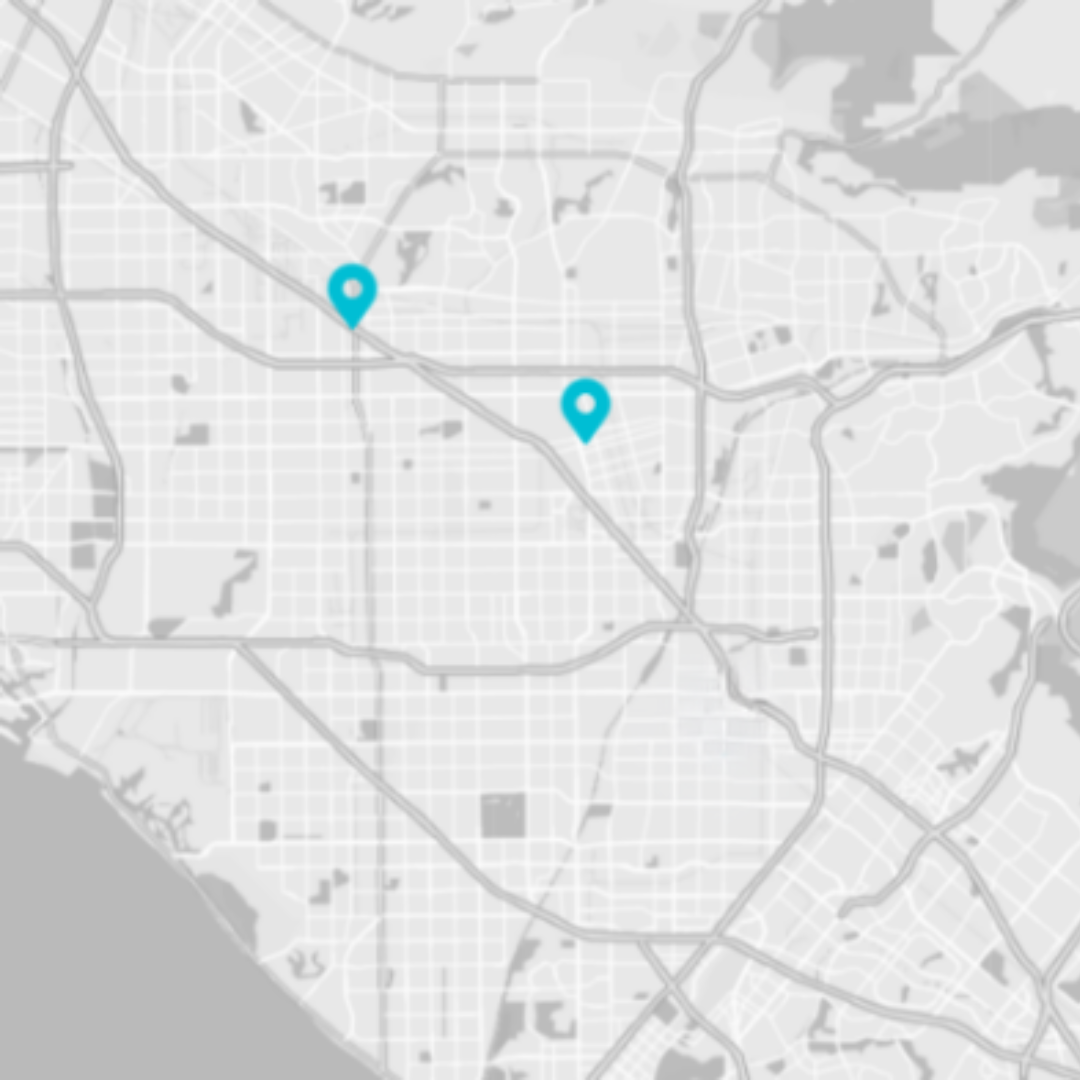
Our Adult Day Services welcome participants in these parts of Central and North Orange County:
Anaheim
1158 N. Knollwood Circle
Anaheim, CA 92801
714.220.2114
Hours: 7:00 a.m. – 4:00 p.m.
Buena Park
8150 Knott Avenue
Buena Park, CA 90620
714.826.3163
Hours: 8:30 a.m. – 4:00 p.m
What We Provide
Two Meals on Wheels OC Adult Day Services Centers help keep families together by supporting the medical and social needs of adults living at home who need daytime health and safety assistance.
Our Adult Day Health Care center in Anaheim welcomes adults with physical challenges and limitations or dementia conditions. Our caring expert staff offers nursing care, medication management, health therapies, transportation, enriching activities, and nutritious meals that meet dietary and cultural needs and preferences. Transportation to and from the center is also available.
Cost: Covered by Cal Optima PACE, Medi-cal, Veterans Administration, and private pay.
Our Adult Day Services in Buena Park provides caregiver respite and social opportunities, mental and social stimulation activities, physical fitness, nutritious meals, and friends for adults with dementia, memory loss, or behavioral conditions needing a healthy, loving environment during the day.
Cost: We kindly request a voluntary contribution of $45 a day; however, individuals will not be refused services for their inability to contribute.
*Buena Park Adult Day Services is licensed by the California Community Care Licensing Division and funded in part through a grant from the Department of Aging as allocated by the Orange County Board of Supervisors and administered by the Office on Aging.


What We Provide
Two Meals on Wheels OC Adult Day Services Centers help keep families together by supporting the medical and social needs of adults living at home who need daytime health and safety assistance.
Our Adult Day Health Care center in Anaheim welcomes adults with physical challenges and limitations or dementia conditions. Our caring expert staff offers nursing care, medication management, health therapies, transportation, enriching activities, and nutritious meals that meet dietary and cultural needs and preferences. Transportation to and from the center is also available.
Cost: Covered by Medi-cal, Veterans Administration, and private pay.
Our Adult Day Services in Buena Park provides caregiver respite and social opportunities, mental and social stimulation activities, physical fitness, nutritious meals, and friends for adults with dementia, memory loss, or behavioral conditions needing a healthy, loving environment during the day.
Cost: A suggested donation is encouraged

Who Qualifies
We welcome individuals who are living with a physical or mental impairment that handicaps daily life. They must have the capacity to improve or maintain physical and mental health, so that they can achieve or maintain independence.

Who Qualifies
We welcome individuals who are living with a physical or mental impairment that handicaps daily life. They must have the capacity to improve or maintain physical and mental health, so that they can achieve or maintain independence.
What Our Clients Have to Say
You can read statistics to see the impact you can have on the clients we serve … but we think our clients explain it best:
Request Adult Day Services
You can call us at 714.220.0224 or, you can fill out this form and we will contact you.









